1890
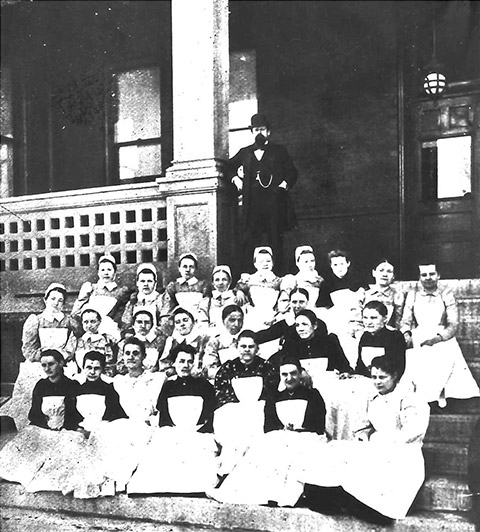
The Protestant Deaconess Society of Dayton is Formed
At its founding, the Protestant Deaconess Society of Dayton provided house-to-house care to serve the rapidly expanding Dayton population.

All Premier Health Urgent Care locations, including virtual urgent care, will be open from 9 a.m. to 3 p.m. on Christmas Day.
At its founding, the Protestant Deaconess Society of Dayton provided house-to-house care to serve the rapidly expanding Dayton population.

The original hospital was housed in a private home and had room for 37 beds. Very soon it became clear that the hospital had overgrown the house, so the Society began fundraising for a dedicated hospital building.
| Date | Image | Description | Link |
|---|---|---|---|
| 1894 |  | Hospital Building is DedicatedThe original hospital was housed in a private home and had room for 37 beds. | |
| 1899 |  | Dayton's First School of Nursing is Established |

| Date | Image | Description | Link |
|---|---|---|---|
| 1912 |  | Opens Dayton’s first emergency room | |
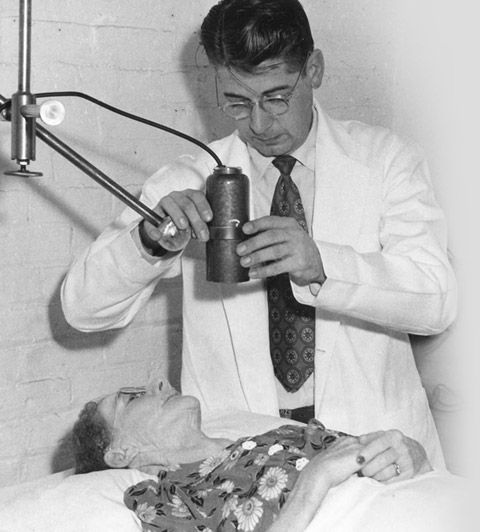
| 1931 | Becomes the National Center for Fever Therapy Research |

Miami Valley Hospital served as the primary care facility for polio until the Salk vaccine was instituted in 1955.
Photo Credit: FDR Presidential Library & Museum photograph by Margaret Suckley
| Date | Image | Description | Link |
|---|---|---|---|
| 1948 | Opens the Region’s First Hospital-Based Psychiatric WardAt this time, fewer than 1% of American general hospitals offered inpatient psychiatric services. |

MVH aimed to build a modern, efficient building which allowed for further expansions in the future. The fundraising effort was the largest civic undertaking in Dayton history at this time.
MVH was the first non-university hospital in Ohio to be authorized by the Atomic Energy Commission to use radioactive materials in research and patient care.
| Date | Image | Description | Link |
|---|---|---|---|
| 1959 | Opens Dayton’s First Intensive Care Unit | ||
| 1965 | MVH’s First Coronary Care Unit is Established |
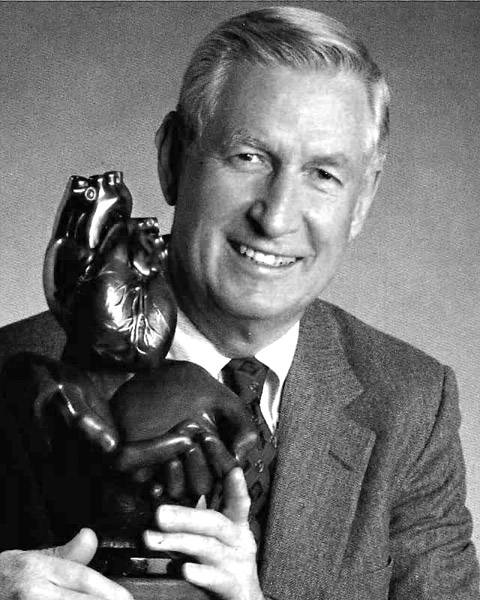
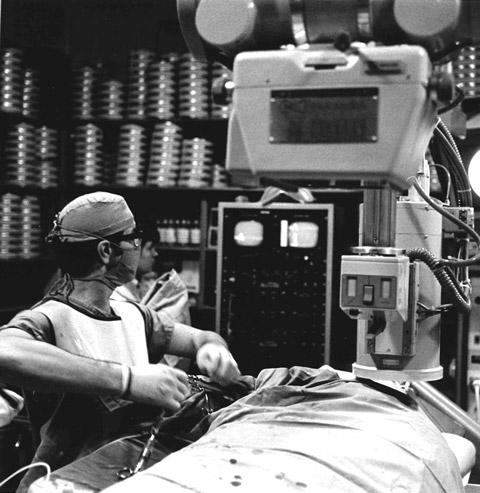
After the establishment of the Cardiac Catheterization Lab in 1957, MVH continued to expand their cardiac technologies. Dr. Kenneth Oberheu performed the first open heart surgery on November 28, 1968.
| Date | Image | Description | Link |
|---|---|---|---|
| 1974 | Federal Government Designates MVH as Regional Treatment Center for Kidney Dialysis | ||
| 1975 | MVH’s NICU Attains Highest Level of Care (Level III) for High-Risk Obstetrical and Newborn Care |

| Date | Image | Description | Link |
|---|---|---|---|
| 1991 | MVH Campus Becomes Smoke-Free |


MVH and Good Samaritan (closed in 2018) join together to create an integrated network that will offer the most comprehensive continuum of health care services in the region.
The new facility houses the Shaw Emergency and Trauma Center, an updated Surgical Center and related medical and support services.
| Date | Image | Description | Link |
|---|---|---|---|
| 1998 | MVH Serves More Than 34,000 Inpatients, a Record | ||
| Jan 2000 | The First Set of Quintuplets are Born in the U.S. in the New Millennium |

The project provides opportunities and financial incentives to MVH employees to purchase homes in the Fairgrounds neighborhood.

| Date | Image | Description | Link |
|---|---|---|---|
| 2002 | Earns the Region’s No. 1 Heart Program Rating by HealthGrades | ||
| 2002 | MVH is Ohio's Busiest Emergency Department With 95,878 Visits this Year |


The ANCC’s Magnet Recognition Program recognized that MVH met its stringent quality and professional standards, an honor that MVH holds to this day.

| Date | Image | Description | Link |
|---|---|---|---|
| Feb 2004 | Burn Center Celebrates its 30th Anniversary |


| Date | Image | Description | Link |
|---|---|---|---|
| Feb 2008 | Plans for a New Patient Tower are Announced | ||
| July 2008 | Center for Nursing Excellence Moves to a New Location in Weber Center for Health Education |

| Date | Image | Description | Link |
|---|---|---|---|
| June 2009 | Miami Valley Hospital South Expands | ||
| Aug 2009 | 1,000th Robotic Surgery is Performed at Miami Valley Hospital |
The new institute both benefits patients with a variety of neurological disorders and attracts funding for advanced biomedical research to the Dayton area.

MVH acquires new technology to help treat stroke and aneurysm victims, including the Solitaire Revascularization Device and Pipeline Embolization Device.


A new spine and joint center, maternity services and the announcement of a new comprehensive cancer center help MVH continue to deliver award-winning services.


| Date | Image | Description | Link |
|---|---|---|---|
| Jan 2013 | Comprehensive Cancer Center Opens | ||
| Mar 2013 | MVH Opens Emergency Center in Jamestown |
Today, the CareFlight program serves over 150 hospitals and over 300 community fire and police departments in 17 counties. Since its inception, CareFlight has made over 25,000 flights.
| Date | Image | Description | Link |
|---|---|---|---|
| Feb 2014 | Miami Valley Hospital Emergency Department Renovation is Completed |

From modest beginnings more than 100 years ago as a 37-bed hospital housed in a converted private home, Miami Valley Hospital (MVH) has grown to an 848-bed regional referral and specialty center.