Uniquely Female
As a woman, your health needs change throughout your life. Get guidance from the Premier Health providers you can trust. Their reliable information covers every stage of your life to ensure you’ll recognize when your health may be at risk, and how to get the care you need.
Menopause
Endometriosis

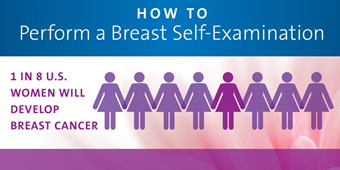
- Cancer Information for Women
- Endometriosis
- Getting Pregnant
- Health Topics
- Infertility
- Uniquely Female
What you need to know for your good health.